How Periodontal Disease Makes COVID-19 Worse
Aging with a Vengeance is more than gaining muscle mass and losing fat around your waist; it also means that your immune system is robust. I think we often over-emphasize supplementation; while I think it’s necessary, it really should serve as support for other actions that are equally or even more important. For example, taking care of your teeth. By that, I mean regular checkups, brushing after meals, and flossing every day. Does that affect the immune system? You bet it does, and a recent study illustrates how significant that can be.
Researchers in Qatar conducted a study to see if people with periodontal disease had an increased risk of being in the intensive care unit (ICU), being put on a ventilator, or dying from COVID-19. Qatar Is a country of 2.3 million people with an advanced electronic medical records system; because dental records are a part of the medical records system, they were able to identify people with periodontal disease, sometimes called gum disease. In addition to the medical records on COVID-19 and how the subjects fared, they were also able to get data such as BMI, HbA1c, and CRP, among other health indicators.
As an observational study, researchers were able to find 568 people who were diagnosed with COVID-19 between February 2020 and the end of July. That number included 40 people with severe cases of COVID-19 that required hospitalization. The characteristics of those who had severe cases are similar to what we find in the U.S.: more were overweight or obese, had higher HbA1c levels, and had higher CRP levels.
Of those who had periodontal disease, 33 had severe cases of COVID-19; only seven people who had no periodontal disease had a severe outcome. When looking at the odds ratios, a person with periodontal disease had six times the risk of being admitted to the ICU, almost eight times the risk of being put on an ventilator, and a 17 times greater risk of death from COVID-19.
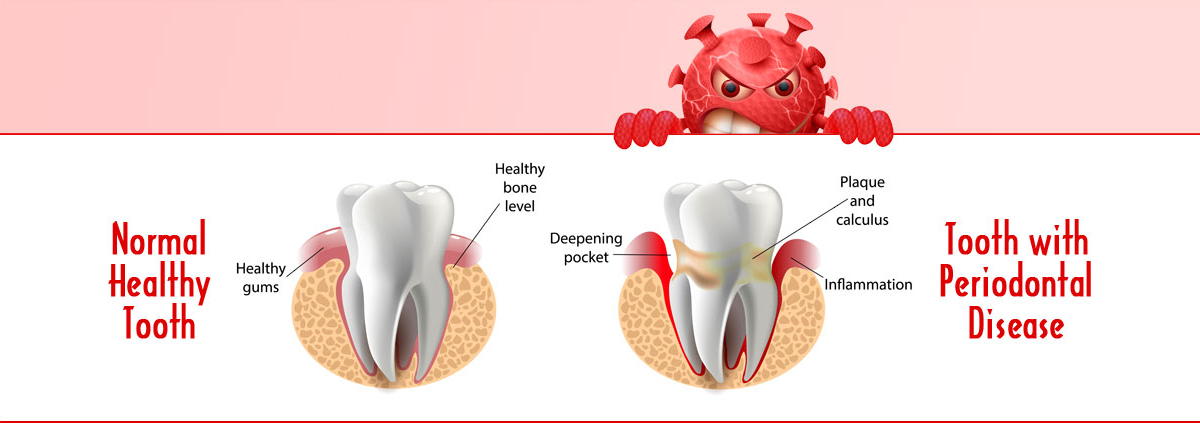
Why would having periodontal disease, an infection that appears to be limited to the teeth and gums, have such an overall effect? The reason is that it creates a state of higher inflammation that compromises the immune system. When exposed to the virus, the immune system is already stressed and the body does not have all the resources it needs to fight the infection.
The Bottom Line
Here’s my advice: if you’re overdue for your dental checkup, call and make the appointment, especially if your gums bleed regularly when you floss, if your gums seem inflamed, or if you have a very bad mouth odor. No excuses; gum disease should not be ignored.
I see many comments in social media about “all the talk being about vaccinations, masks, and social distancing.” “No one ever talks about diet and exercise, etc.” The reason, at least in my humble opinion, is that the last 50 years have clearly demonstrated that most people in the U.S. don’t eat well, don’t move enough, and eat more than they should.
Instead of criticizing people for their poor dietary and exercise habits, the current medical approach seems to be to meet people where they are. My hope is that by addressing some of the other issues related to health, such as periodontal disease and overall healthcare in our quest to age with a vengeance, all readers will see ways to make their immune system much more robust so it can do a better job of protecting them.
And if it has the side benefit of shutting up the naysayers that talk about long-term solutions only at the exclusion of the things that we know are working right now—such as vaccinations, masks, etc.—I’m good with that. As I said in May, not fear; respect.
What are you prepared to do today?
Dr. Chet
Reference: J Clin Periodontol. 2021. DOI: 10.1111/jcpe.13435.