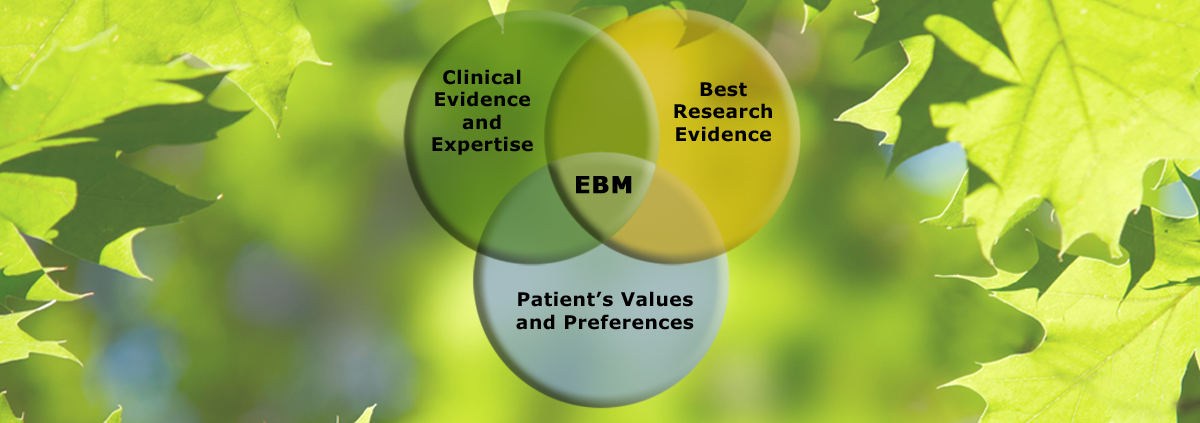
What Is Evidence-Based Medicine?
The term evidence-based medicine (EBM) dominates the scientific literature related to the treatment of disease. In short, the use of EBM is intended to treat patients based on the best available science and research; only the largest, best designed, and strongest studies are used when setting up the standards for treatment. That seems to make sense. That applies to the use of medications for the treatment of type 2 diabetes in adults as well as other diseases.
In the past, physicians primarily depended on their training. It doesn’t mean they didn’t use science to guide their decisions, but where and how physicians were trained influenced their treatment decisions more than research and science. That’s why EBM was developed; the use of solid evidence when considering treatment of patients keeps treatment up to date.
The problem is that the way EBM evolved appears to have excluded one of the primary purposes of how it began: consideration of the values and preferences of the patient. Treating patients should never be a one-way street. Your doctor should be a trusted advisor, not a dictator, and should give you the most up-to-date options for treatment of your condition; then you decide together which treatment option fits your life. The clinical and research evidence guides the physician in what to do along with knowledge of your personal health history, but only in the context of what you want.
For example, if after discussing all the options, a patient decides an earlier death is preferable to extending life by taking medication and suffering horrible side effects, that’s a valid preference that the doctor must respect. Another example: if the patient’s life expectancy is less than 10 years or so, pain management may be a better option than joint replacement when all the ramifications of major surgery are considered. That kind of joint decision-making is what EBM is supposed to be all about.
Saturday I’ll look at the guidelines for HbA1c proposed by the American College of Physicians in light of EBM. It’s a Memo you don’t want to miss.
What are you prepared to do today?
Dr. Chet
Reference: Ann Intern Med. doi:10.7326/M17-0939.